How Fasting Works
Simple science, practical takeaways.
Fasting changes more than your eating schedule it changes how your body fuels, repairs, and regulates itself. Here are the key processes explained simply:
Metabolic Switching & Signalling
Circadian Timing (Biological Clock)
Autophagy (Cellular Housekeeping)
Longevity Angles
Weight & Metabolic Health
Details are Given Below
One
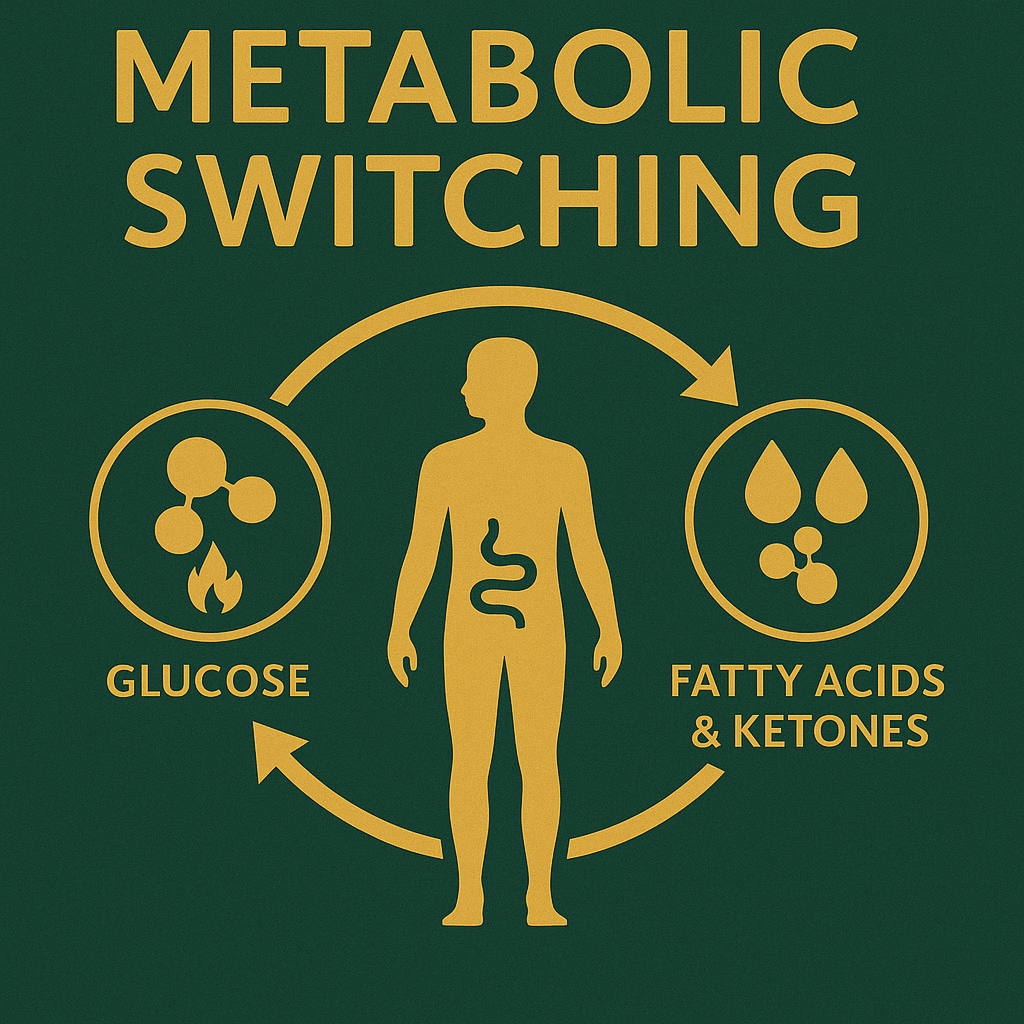
Metabolic Switching & Signalling
When you fast long enough, your body gradually shifts away from burning glucose as its main fuel. Instead, it starts using fatty acids and ketones. This process, often called metabolic switching, activates signalling pathways like AMPK and mTOR, which play roles in energy regulation and repair (Mattson).
What it means for you:
Fasting encourages your body to become more flexible in how it uses energy, which may improve resilience and reduce energy crashes.
Two
Circadian Timing (Biological Clock)
Your body has a natural clock that governs sleep, hormones, and metabolism. Eating in sync with this clock matters. Research by Satchin Panda shows that earlier eating windows—finishing meals earlier in the day—can improve blood sugar control and appetite regulation, even without weight loss.
What it means for you:
Eating earlier in your fasting rhythm may help you feel more balanced and support metabolic health.
Two
Circadian Timing (Biological Clock)
Your body has a natural clock that governs sleep, hormones, and metabolism. Eating in sync with this clock matters. Research by Satchin Panda shows that earlier eating windows—finishing meals earlier in the day—can improve blood sugar control and appetite regulation, even without weight loss.
What it means for you:
Eating earlier in your fasting rhythm may help you feel more balanced and support metabolic health.
Three
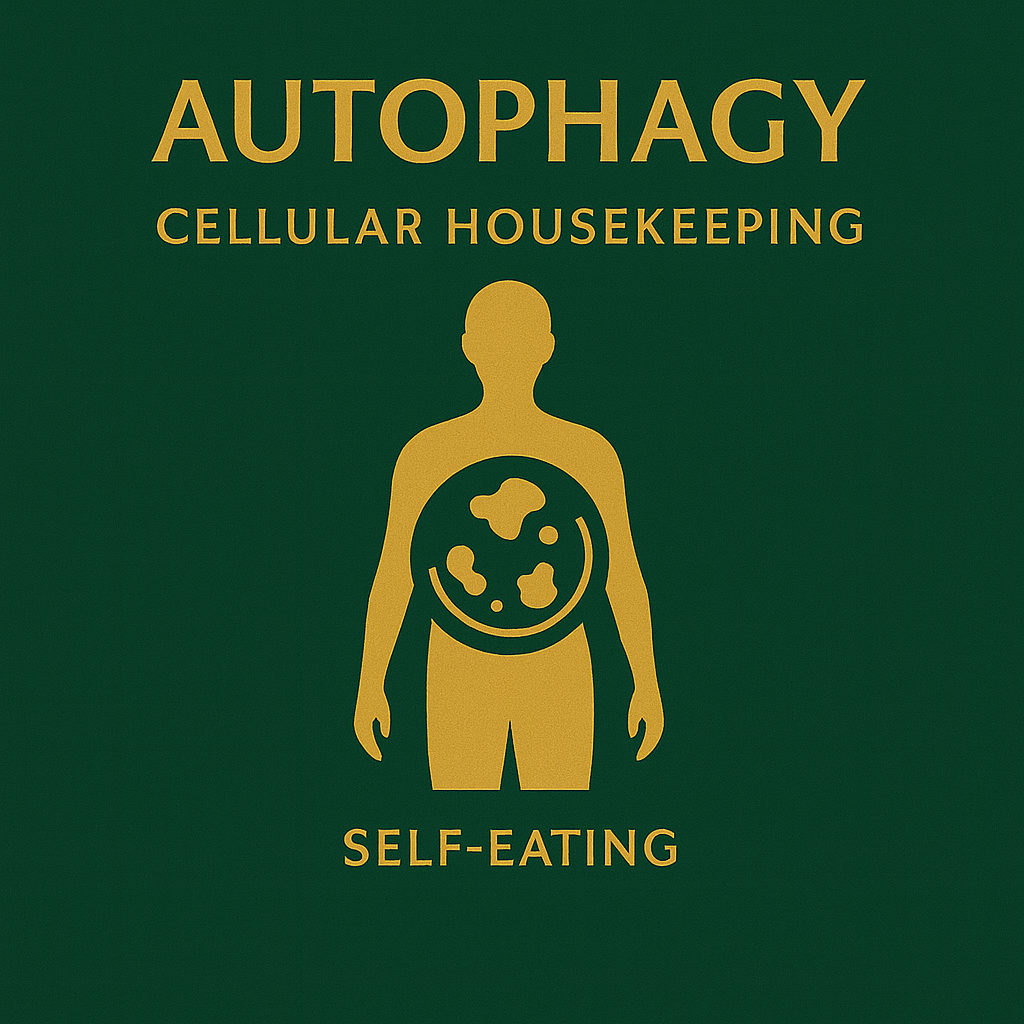
Autophagy (Cellular Housekeeping)
In longer fasts, your cells enter a process called autophagy, which literally means “self-eating.” Damaged proteins and cell components are broken down and recycled. Yoshinori Ohsumi’s Nobel Prize–winning work put autophagy in the spotlight. This process supports cellular repair, resilience, and healthy aging.
What it means for you:
While autophagy is promising for longevity, it’s not a license for extreme fasting. Balance and safety still matter most.

Weight & Metabolic Health
Four
Large studies comparing intermittent fasting with continuous calorie restriction often show similar weight-loss results. The biggest factor isn’t the method—it’s sustainability. Individual responses vary widely. What truly matters is finding an approach you can stick with long term.
What it means for you:
The “best” fasting protocol is the one you can keep doing while maintaining food quality, sleep, and lifestyle balance.
Four
Weight & Metabolic Health
Large studies comparing intermittent fasting with continuous calorie restriction often show similar weight-loss results. The biggest factor isn’t the method—it’s sustainability. Individual responses vary widely. What truly matters is finding an approach you can stick with long term.
What it means for you:
The “best” fasting protocol is the one you can keep doing while maintaining food quality, sleep, and lifestyle balance.
Five
Longevity Angles
Valter Longo’s Fasting-Mimicking Diet (FMD) explores periodic fasting designed to trigger healthy-ageing biomarkers. It’s an exciting area of research, but it’s a specialist protocol—not suitable for everyone. Always approach it with guidance and medical oversight.
What it means for you:
Fasting may support long-term health, but daily habits and safety should always come first.
The Fasting Treasure No where to found

Intermittent Fasting for Type 2 Diabetes: Remission, Meds, and Real-World Practice
Type 2 diabetes (T2D) is fundamentally a carbohydrate-intolerance disease driven by insulin resistance and excess liver/visceral fat. Intermittent fasting (IF) can attack each mechanism by lowering basal insulin, improving insulin sensitivity, and shrinking ectopic fat—sometimes allowing medication reductions under medical supervision.
What the evidence shows
Intermittent energy restriction vs. continuous restriction. In adults with T2D, intermittent energy restriction (e.g., 5:2) achieved non-inferior HbA1c reductions and weight loss compared with continuous daily restriction over 12 months (Carter et al., 2018).
Time-restricted eating (TRE). Early TRE improves glycemic variability and insulin sensitivity even without weight loss in prediabetes (Sutton et al., 2018). TRE studies in people with metabolic syndrome show lower 24-hour glucose, smaller post-meal excursions, and improved blood pressure (Wilkinson et al., 2020).
Medication de-intensification (clinical experience + small trials). Many patients can reduce insulin or sulfonylureas when fasting windows begin—only with clinician oversight to avoid hypoglycemia. GLP-1 receptor agonists and metformin pair well with IF but still warrant monitoring.
Why IF works in T2D
Lower insulin exposure (fasts) restores receptor sensitivity.
Hepatic fat reduction improves hepatic insulin signaling and fasting glucose.
Improved metabolic flexibility reduces post-prandial spikes; ketone signaling may calm inflammation that drives insulin resistance.
Earlier windows leverage circadian biology—your pancreas and muscles handle calories better earlier in the day.
Practical T2D IF framework (with clinician)
Pick a gentle start: 12:12 for 1–2 weeks (no food 8 pm–8 am). Track fasting glucose and symptoms.
Progress to 14:10 or 16:8, ideally ending meals earlier (e.g., 8 am–6 pm or 10 am–6 pm).
Meals in the window: protein-forward, high-fiber, minimally processed carbs, healthy fats.
Movement after meals: 10–15 minutes walking lowers post-prandial glucose.
Strength training 2–3×/week: increases GLUT-4 and insulin sensitivity.
Medication plan: pre-agree with your clinician how to titrate insulin/sulfonylureas on fasting days to prevent hypos.
What about remission?
Large remission trials using low-energy diets (e.g., DiRECT) show substantial diabetes remission with weight loss driven by calorie restriction and liver/visceral fat loss. IF is a different structure to create similar energy deficits and fasted signaling. Remission depends on magnitude of fat loss and duration; IF can be the sustainable method that gets you there.
Safety and red flags
Do not begin aggressive fasting while on insulin or sulfonylureas without a medication plan.
Be cautious with SGLT2 inhibitors (risk of euglycemic ketoacidosis in rare cases) if combining with prolonged fasts.
If you experience hypoglycemia, dizziness, or confusion, break the fast and follow your clinician’s plan.
Pregnant/breastfeeding: IF for weight loss is not appropriate.
Bottom line
IF can be a powerful adjunct for T2D: lower insulin exposure, better glycemic profiles, weight and visceral fat loss, and potential medication de-intensification—when done safely with clinician guidance and anchored by protein-rich, fiber-dense meals and regular movement.
Selected references
Carter S et al. Intermittent vs continuous energy restriction in T2D. JAMA Netw Open. 2018;1:e180756.
Sutton EF et al. Early TRE in prediabetes. Cell Metab. 2018;27:1212–1221.e3.
Wilkinson MJ et al. TRE improves cardiometabolic health in metabolic syndrome. Cell Metab. 2020;31:92–104.
de Cabo R, Mattson MP. N Engl J Med. 2019;381:2541–2551.
What’s Next Step
Explore our Beginner’s Guide or download the 14-Day Plan to start applying these principles safely in your daily life.

COMPANY
Keep in Touch
Copyrights 2025 | Terms & Conditions
Disclaimer: The information available is for informational purpose only and not intended to diagnose, treat, cure, or prevent any disease.